BMI’s predictive analytics support physicians to identify and stratify patients based on their current and anticipated level of health care needs; engage and activate them through BMI’s proprietary technology platforms to provide the support they need to self-manage their condition.
Care Management Programs
BMI assists physicians and practices in optimizing their revenue generation from Medicare and related programs. For these programs, physicians and practices retain control and responsibility of their patients while BMI simply provides the care coordination services and non-face-to-face encounters of the patients enrolled in the programs.
Program Goals
- Develop patient self-management skills
- Improve the patient experience of care
- Reduce ER and inpatient utilization
- Improve patient’s functional health status
- Enhance coordination of care
- Eliminate duplication of services
- Reduce the need for costly medical services
- Reduce the per capita cost of health care
Our Approach
BMI screens enrollees early for co-morbidities or complications and aimed at managing total population health. Medicare beneficiaries with co-morbidities and complications are frequently assigned to higher care levels and receive more intensive attention. Beneficiaries who suffer from multiple conditions often receive care coordination and related services. BMI’s programs are designed to manage disease states that tend to occur together. For example, asthma patients may be diagnosed with a chronic obstructive pulmonary disease (COPD) which may be due to smoking, and chronic heart failure may emanate from a complication of diabetes.
Programs Features
- Face-to-face encounter as a supplement to telephone encounters
- Multidisciplinary care teams, including registered and licensed practical nurses (RN/LPN)
- Physician involvement and consultation.
- Patients with complex healthcare needs, those suffering from physical or cognitive functions are assigned to informal caregivers.
- Patient engagement and coaching activities to help with identifying early warning signs of worsening disease states and to adopt self-care habits to improve health management
- Remote patient monitoring and telehealth services to avoid exacerbations.
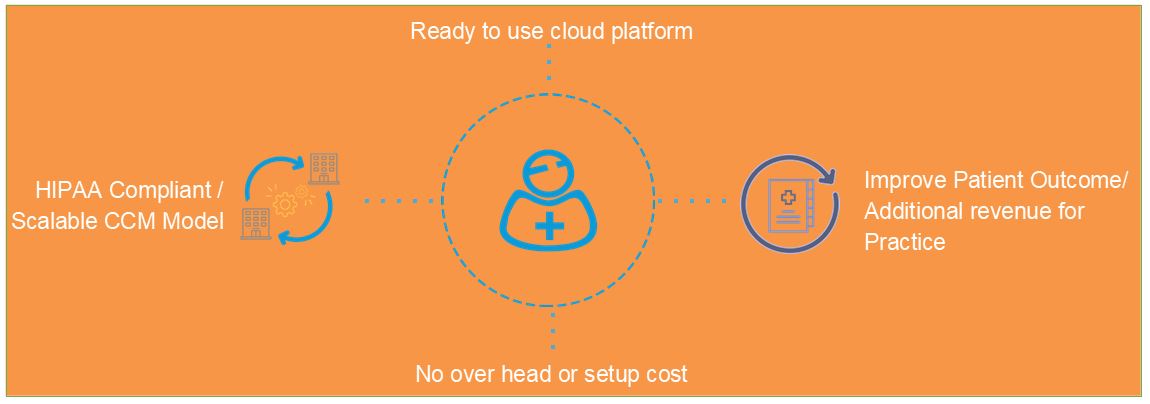
Why BMI Platform?
- Create condition-specific care plan for patients using
Care Assessment - Reduce documentation time and increase
Productivity and Provide Quality care….
- Billing Reports based on CMS guidelines
for Guaranteed Reimbursement
Key Features of BMI’s CCM Technology Platform
- 24/7 care plan access using secured cloud platform
- Claims/billing data integrations
- Analytics to identify and monitor CCM qualified members
- Comprehensive Care assessments
- Individualized plan of care (Issues, Goals, and Interventions)
- Secure messaging
- Provider/ Patient Portals
- Patient Mobile App
- Report Engine to create custom reports for Billing and Productivity
- Softphone Integration with In-app calling
- Workflow engine to create custom workflows for Care coordinators/care managers
- Daily work queue
- Patient dashboards
- Patient-level comprehensive clinical profile
- Session notes / Service Logs
- Integration with leading EMR
- Multi-tenant – Manage multiple practices under one roof
- MIPS/MACRA Dashboard
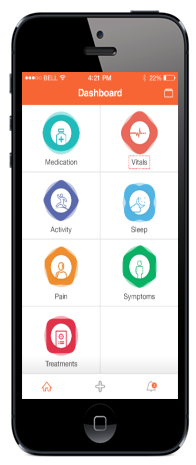
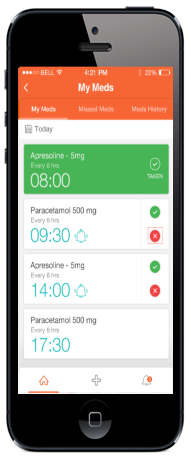
Patient Mobile App
Native Patient App – A native patient app that can record medication compliance, record daily vitals and track pain, activity, sleep, and symptoms
Get Started Today! Call 201-428-9090.